Since its inception, the Samuel Proctor Oral History Program has been an ally and resource for older persons, from its home base at UF to the far corners of the globe. Not only does SPOHP provide narrators the adequate time and space, in a world so full of speed and sound bites, to tell history as they have encountered it, but it does so with the promise that their recordings will be securely stored and readily accessible to friends, family, and scholars. Oral history also gives interviewers a chance to learn the lost art of listening through hands-on practice with the latest advances in digital technology.
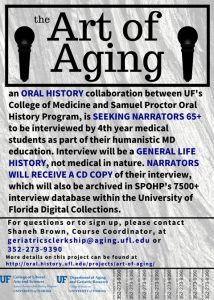
In the summer of 2017 SPOHP was approached by Nina Stoyan-Rosenzweig, Archivist and Education Coordinator at UF Health Science Center Libraries, and Dr. Mallory Otto, Clinical Assistant Professor at the UF College of Medicine, to develop an oral history segment for the Geriatrics Medicine Clerkship, a required rotation for all 4th year medical students that Dr. Otto directs. SPOHP’s Ryan Thompson took on leadership for its half of the partnership. This marked the beginning of another significant partnership for SPOHP, one of many individual and organizational collaborations over the program’s half-century existence. Collaborations like these have proven mutually beneficial for SPOHP and its partners in professional and academic fields and beyond.
“Medical science has one approach to saving lives, and oral history has another by documenting and preserving each individual’s history.” – Deborah Hendrix
A core goal of the Geriatrics Clerkship is “to understand how to talk to older patients,” which is a skill set that SPOHP is especially well-suited to enhance. The clerkship is designed to “to promote self-directed learning.” Furthermore, it is “also is designed to create a humane environment that fosters respect, personal integrity, service orientation and a sense of personal well-being” and adheres to the ethos that “Caring for older patients takes time.” Students “are expected to treat their patients with respect, compassion and humility as if they were treating their own family members.” All of these values are shared with SPOHP, and a natural affinity between the programs quickly emerged.
Beginning in September 2017 with a group of sixteen medical students, SPOHP began to train those on their Geriatrics Clerkship rotation in the art and science of oral history, from its interdisciplinary methodology to interviewing skills to the use of technology and equipment. Students began by meeting with Deborah Hendrix, SPOHP’s Digital Humanities Coordinator, who gave a demonstration on the use of the Marantz recorder they bring with them into the field, as well as an overview of the Deed of Gift that narrators fill out and sign to grant SPOHP rights to the recording. Having gotten a tactile introduction to the process, including touring SPOHP’s physical archives in Pugh Hall, students participated in a workshop led by SPOHP staff and longtime volunteers, who have included Susan Atkinson, Ebony Love, Jennifer Romero, Sandra Romero, Ann Smith, and Ryan Thompson. Skills covered include active listening and, specific to this audience, differentiating between the “social histories” that clinicians grow accustomed to (“Please check if you have ever had any of the following”) and the life histories that SPOHP gathers, preserves, and promotes. Students are reminded that a good interview is a guided conversation and that simple, open-ended questions are best for oral history interviews. Following their workshop, students visited Oak Hammock to meet and interview narrators. (Sites will expand over time, and recently narrators have begun to be recruited in collaboration with Gainesville’s grassroots Community Coalition for Older Adults). Within a few days of their interview, each pair of students gives a presentation featuring audio vignettes from it as well as their impressions of the process.
“Stories help to put patient values into perspective, and when often medical ailments can dominate day to day life as people age, this helps to frame a clinical focus as well.” – Dr. Mallory Otto
Over the Fall 2017 semester, 39 medical students completed the training and interviewed 20 narrators who reside at Oak Hammock. Stoyan-Rosenzweig, Otto, and Thompson will present initial findings of this project, specifically its benefits to medical education, at the 2018 International Health Humanities International Health Humanities Consortrum Conference held at Stanford University.
Providing anonymous feedback following their three-day immersion in oral history, students have generally lauded the experiential learning opportunity as one that keeps them grounded in humane medicine. A student from one of the first periods to have gone through the oral history segment to the Geriatrics Clerkship said that the “opportunity to meet and get to know someone, especially an elderly person with so much life experience, outside of just their medical history was very enjoyable. I also think the people we interviewed appreciated the opportunity to talk about themselves and be listened to. . . .” Another stated that “this was something different than what we normally do on the wards. It was refreshing to do something new outside of the . . . academic medicine setting. . . .” Such sentiment parallels what physician-author Danielle Orfi has written about the transition in medical school from the classroom years to the clinical years: “Many of the qualities that students entered medical school with—altruism, empathy, generosity of spirit, love of learning, high ethical standards—are eroded by the end of medical training. Newly minted doctors can begin their careers jaded, self-doubting, even embittered (not to mention six figures in debt.)” One student embraced the chance to spend “actual time” with an older person and hear their story and another “loved hearing the interviewee tell his story and hearing the other stories during the class.”
“. . . our elders have a lifetime of experiential knowledge that we could learn from if we knew how to get it. They are at a stage of life where they are reflecting on their past and many times welcome a large boost to documenting values they would like to pass on.” – Ann Smith
“Listening to someone describe their first day at work, school days, participation in unofficial strikes, childbirth, courtship, housework, historians have learned to broaden ideas of what history is about,” wrote Joanna Bornat in “Oral History as a Social Movement: Reminiscence and Older People.” Listening to such stories can also broaden clinicians ideas of what medicine is about. Dr. Sayantani DasGupta of the Program in Narrative Medicine at Columbia University writes of the potential benefits of incorporating oral history into medical training to “allow learners to witness stories in profound and potentially transformative ways, even as they witness their own processes of witnessing. By placing the interviewer in the position of self-reflective learner, oral history suggests for clinicians a radically different stance from which to approach storytellers. Ultimately, these exercises can inspire not only a deeper understanding of the self and the other, but advocacy and action.” Clinical psychologist Alan Dienstag and author Don DeLillo’s writing groups for people in the early stages of Alzheimer’s disease, the Veterans Health Administration’s “My Life, My Story” project, and the Reflections: Hospice of the Bluegrass Oral History Collection at the University of Kentucky are but a few sources of inspiration for this collaboration between SPOHP and the Geriatrics Clerkship.
Oral history has an interdisciplinary nature, and the same is true of geriatric medicine. Students in this clinical rotation are trained to be members “of an interdisciplinary healthcare team which develops personalized care . . . for each patient. . . .” In this nascent partnership between the Samuel Proctor Oral History Program and the Geriatrics Clerkship, many skills and styles are valued and coordinated, not only to collect and archive interviews but to improve medical education. Perhaps the best anecdotal evidence of the relevance of this partnership so far have been the narrators, some of whom were eminent members of the healthcare profession, who comment on the “soft skills” that oral history training and practice imparts, and students who note that their core belief that medicine is a humanistic calling has been revitalized. Some clips in which narrators address what they value most in physicians are featured below.
These are some of the individuals who have brought countless skills and backgrounds to this collaboration:
Ann Smith
Smith was an active leader in nursing and nursing education at UF and the North Florida Regional Medical Center in the late 1960s when nurses began to be acknowledged as more than “secretaries” who brought coffee to doctors, but as skillful healthcare professionals in their own right. Since “retiring,” Smith has volunteered thousands of hours of her time to SPOHP, where she coordinates the Veterans History Project and now helps lead trainings for the Geriatrics Clerkship.
Of SPOHP’s collaboration with the Geriatrics Clerkship, Smith says “ . . . our elders have a lifetime of experiential knowledge that we could learn from if we knew how to get it. They are at a stage of life where they are reflecting on their past and many times welcome a large boost to documenting values they would like to pass on. The older generation are often excluded in our society and feel it a great honor to be asked about their personal stories. For most of us, an oral history is a win-win—we gain insight into a time and place and they gain the acknowledgment that we respect the lives they have lived.”

Deborah Hendrix
Hendrix has worked for SPOHP since 2000 and is the program’s Digital Humanities Coordinator. In a “past life” before her long tenure at SPOHP, Hendrix worked in health care, in hospital laboratories as a medical technician. Hendrix is responsible for managing SPOHP’s collection of 7,500+ oral history interviews and making them publicly accessible.
Of SPOHP’s collaboration with the Geriatrics Clerkship, Hendrix says “This unusual collaboration cannot be anything short of amazing, as I am sure time will tell.”

Ebony Love
While she was still an undergraduate Love found oral history to be a critical tool in her education and has been able to communicate her knowledge as a co-facilitator in workshops training medical students on working with oral history. During the Spring 2017 semester she completed SPOHP’s internship on African American and Latinx Histories, honing many of the skills she would later share with medical students. Love’s interdisciplinary interests are resonant with those of the Geriatrics Clerkship: one among them is the existence of health disparities in society.
Of SPOHP’s collaboration with the Geriatrics Clerkship, Love says “Oral history is a way of revolutionizing history in order to fill in the blanks that traditional historical methods leave open. Working with the elderly population fills in the day-to-day narrative that thematic historical accounts intentionally leave out.”

Ryan Thompson
Coming to SPOHP on a Graduate Assistantship while a graduate student in UF’s Department of History, Thompson has remained on staff at the program while his academic interests shifted. Now an MSW student at Florida State, the topical interests he was able to explore at UF while working with advisors Jack Davis and Joseph Spillane—particularly on changing attitudes toward aging and death in the U.S.—have come full-circle as he focuses on end-of-life social work and helps coordinate the oral history segment of the Geriatrics Clerkship.
Of SPOHP’s collaboration with the Geriatrics Clerkship, Thompson says “The other day in a course I am taking called Caregiving in Later Life, an undergraduate colleague introduced himself to the others in the room by saying that he added a public health minor to his premedical major because all of the necessary scientific training left him feeling estranged from the human side of medicine which drew him to the field in the first place. Medical school students are perhaps given more exposure to the humanistic qualities of medicine than this younger student was receiving in his education, but I have nonetheless felt proud to be a part of this small effort to bring together aspiring clinicians with elders who want to share their stories in such a way that is beneficial to all involved.”

Dr. Mallory Otto
Dr. Otto is the Clerkship Director of the Geriatric Clerkship in the University of Florida College of Medicine.
Of SPOHP’s collaboration with the Geriatrics Clerkship, Otto says “As a geriatrician, I value the endless opportunities to connect with patients through their stories and the opportunity to hear bits of their life narrative and personal experience with historical moments. Stories help to put patient values into perspective, and when often medical ailments can dominate day to day life as people age, this helps to frame a clinical focus as well. I am enthusiastic about highlighting the richness of this opportunity with the field of Geriatric Medicine to burgeoning student-doctors.”

Nina Stoyan-Rosenzweig
Stoyan-Rosenzweig is Co-Founder of the UF & Shands Integrated Arts in Medicine, and Director of the Medical Humanities Program at the University of Florida College of Medicine.
Of SPOHP’s collaboration with the Geriatrics Clerkship, Stoyan-Rosenzweig says “The practice of medicine is ultimately about stories-listening to, interpreting, and understanding stories in order to make a diagnosis, develop a treatment plan, or to connect with a patient. Medical training focuses primarily on the biology of the patient narrative, leaving room for the use of oral history as a means of providing additional interview skills, particularly those that involve connection to the patient. Ultimately, however, the development of oral history interview skills helps students improve their clinical diagnostic skills because they learn more about the individual and the factors affecting their health.”

Narrators
Edward Hutchinson [EOF008] The descendant of several generations of Barbadians, Edward “Hutch” Hutchinson grew up in a working class household in New York City and became a longtime leader at the University of Florida—where he was a professor who trained speech therapists—and in the wider community.
Following his interview Hutchinson wrote the following reflection: “Back in the 70s, when I was on the UF faculty, our Speech Department offered an experimental course on ‘teaching doctors how to communicate with patients.’ We were delighted when some of that year’s Med School graduates who had opted to take that course (certain that it would be a good place to catch up on sleep) reported that it was really very useful to them. My experience two days ago was an absolute hoot. The two young men really seemed to be enjoying the task. I hope they never lose that enthusiasm.”
Jeffery Helicher [EOF016] Born in Philadelphia and serving in the Coast Guard (where his stint included operating a mobile dental detachment) before opening a dental practice in Florida, Helicher spoke in his oral history about the power of listening as an important diagnostic skill in medicine.
Following his interview, Dr. Helicher wrote the oral history project team to note that “I enjoyed my interview with Kaitlyn and Stephen very much. These young students have already developed a nice personal sensitivity and understanding that will help them very much in their careers and also bring credit to your program.”

“The practice of medicine is ultimately about stories- listening to, interpreting, and understanding stories in order to make a diagnosis, develop a treatment plan, or to connect with a patient.” – Nina Stoyan-Rosenzweig